Courtney Stevenson specializes in payor contracting. She has a knack for negotiating contracts with different payers for her clients while maintaining strong relationships on both sides. Through her interactions with clients, as well as experience in previous roles, she has found that good data is essential to helping clients identify deficiencies and opportunities to positively impact their practice. If you’d like to learn more about how Courtney can help you increase your bottom line.
contact her at: cstevenson@datadx.hpamembers.com.
Is your practice receiving the most benefit from the CMS Star Rating System? As the shift towards value-based care models increases and the program continues to gain traction it is highly likely your practice is being affected – whether negatively or positively. If properly adopted, the CMS Star Rating system can help your practice generate additional revenue, help your patients experience better health, and has the potential to increase patient volume. If not utilized to its capacity, the star rating system can impact reimbursement rates from payors and decrease your member panel.
Background
The CMS Five Star Quality Rating System was developed by the Centers for Medicare and Medicaid Services (CMS) to measure members’ experience with their health plans and health providers. According to the CMS website the “purpose of the Quality Rating System (or star ratings) is to:
- Help consumers make informed healthcare decisions,
- Facilitate oversight of health plans, and
- Provide actionable information to health plans to improve the quality of services they provide.”
Program Structure
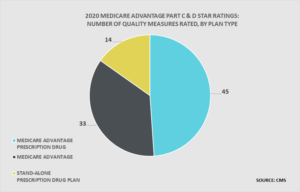
Physician practices are likely most familiar with the star rating program from their participation with Medicare Advantage (MA) plans that offer healthcare services and prescription drug coverage (MA-PD). The highest rating a plan or provider can receive is 5 stars, which indicates a high level of quality of care and allows for prospective members to enroll anytime throughout the year. Ratings are derived from 38 quality measures, belonging to three broader categories listed below. Among the measures are category specific measures which assess the general quality of care provided as well as the members’ experience with their plan.
- Medical Care – This category contributes the most to the overall rating and is based on how well network providers manage member healthcare, how many members receive screening tests and vaccines as well as other basic healthcare services, and management of chronic conditions.
- Members Experience – Based on members’ experience with their plan and member ratings of the care and services received.
- Plan Administration – Scoring is based on how well the health plan is run and ease of access to information, as well as how well network providers facilitate care and appropriate testing.
When health plans earn a high rating they are eligible to earn financial bonuses from CMS. A portion of the bonuses earned through the program are required to be used to improve offerings to members, often in the form of supplemental benefits such as vision or dental coverage. These supplemental benefits not only improve the quality of plans and care available to members, but drive competition in the marketplace resulting in added options.
Practice Impact
The star rating system essentially places providers and plans on the same team, working towards the common goal of patient satisfaction and a high star rating. Physician practices can impact ratings because MA plans are designed to strongly favor clinically integrated networks and reward practices that focus on quality of care and in-network utilization. MA plans offer providers a potential benefit stream above and beyond traditional Medicare when they adopt these practices.
While plans are scored on measures that are more reliant on clinical care than the health plan itself, they can still influence the quality of care provided by encouraging providers to achieve high patient satisfaction. Plans with higher ratings typically see an increase in enrollment as they have access to year-round enrollment versus the end of year traditional enrollment period lower rated plans are limited to. Higher enrollment numbers translate into a larger patient pool, which providers have access to. Health plans pass this revenue on to providers by way of rate increases or incentivizing practices for successful, high quality work.
Setting Your Practice Up For Success
Determining the best strategy for obtaining high ratings can sometimes prove elusive for providers. Practices that adopt an overarching culture with emphasis on patient experience and satisfaction tend to fare better than those who try to focus on specific measures alone to improve their score. The same can be said for health plans. Kaiser Permanent has several plans that scored five stars for 2020. Their company culture champions the star rating program and is structured around data-driven strategies and patient outreach to achieve high ratings. Rather than focusing on individual measures, they implement a more holistic approach with an emphasis on the best long-term outcomes for patients. Clear communication, coordination of care, encouraging members to utilize their covered benefits, and prioritizing the patient experience are all steps that have been taken to improve outcomes.
How can a physician practice contribute to the success of the five-star program and reap the rewards of additional revenue? Physician practices that focus on preventative care and early detection of disease, offer access to programs that help manage chronic conditions, and improve relations with patients will benefit from higher star ratings. Working collaboratively with health plans will also aid in keeping the focus on the patient and continuously improving their experience.